GI switch study—treatment experienced

Study design
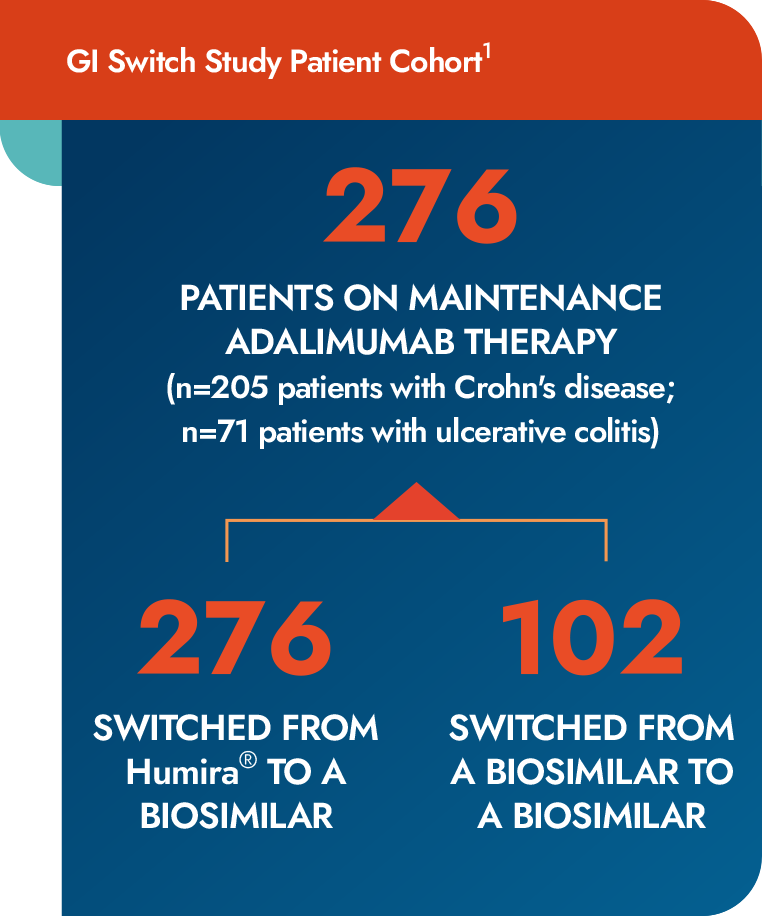
- A prospective study including 276 consecutive patients on maintenance adalimumab therapy (n=205, Crohn’s disease; n=71, ulcerative colitis)
- 174 patients underwent a switch from reference adalimumab to a biosimilar, and 102 patients switched from a biosimilar to another biosimilar
- Data on clinical efficacy, biomarkers, and adverse events were collected at 4 time points: 8 to 12 weeks prior to switch, at baseline/switch, and 8 to 12 weeks and 20 to 24 weeks after switcha
Study objective
- The primary outcomes of the present study were evaluation of clinical disease activity changes and drug sustainability following a switch between adalimumab biosimilars
- Drug survival was evaluated after a median 40-week follow-up
Results
Drug survival was evaluated after a median 40 weeks, with no significant difference between cohorts1
- No significant difference was found in clinical remission rates at any time point in patients switching from reference adalimumab to a biosimilar
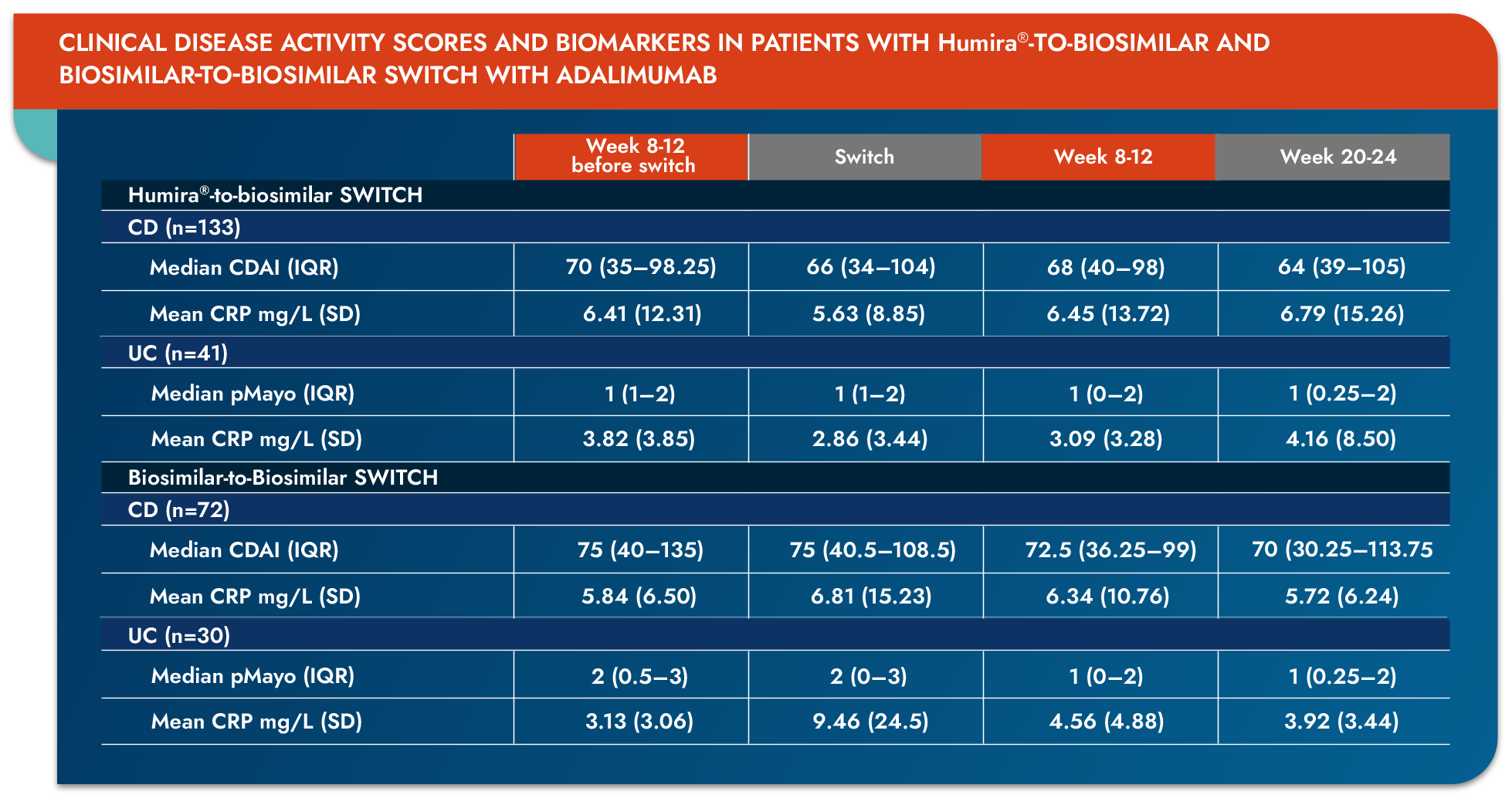
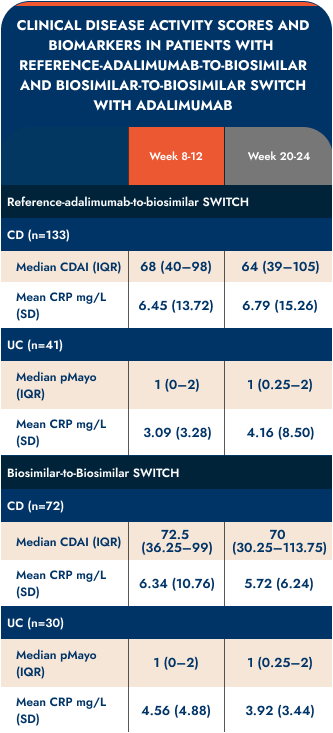
CD=Crohn’s disease; CDAI=Crohn’s Disease Activity Index; CRP=C-reactive protein; IQR=inter-quartile region; pMayo=partial Mayo Score; SD=standard deviation; UC=ulcerative colitis.
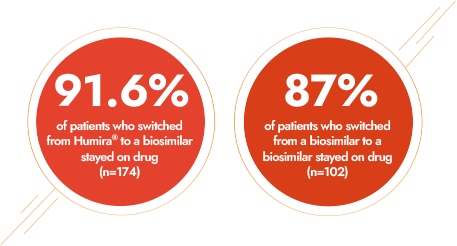
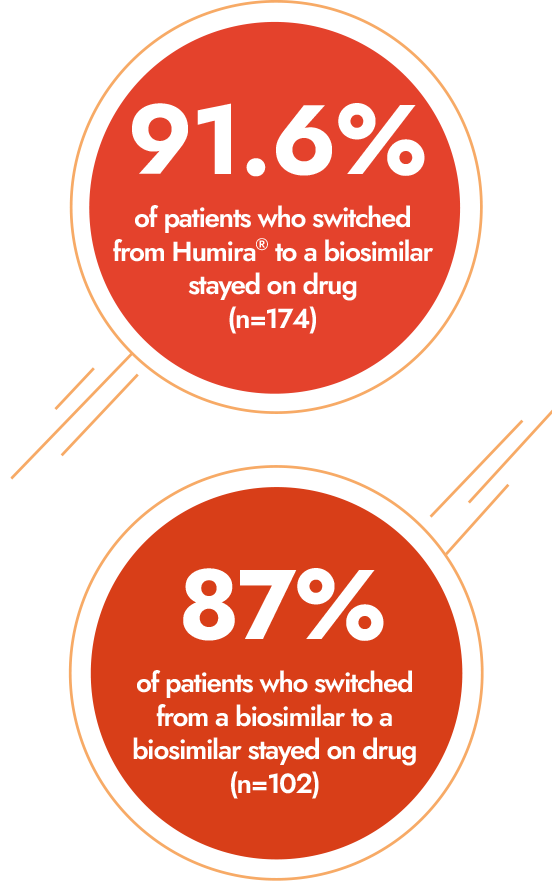
Drug survival was similar between the 2 cohorts after 40 weeks1
- Drug survival was similar between the 2 cohorts, with a probability of 91.6% (reference adalimumab to biosimilar) and 87.0% (biosimilar to biosimilar) to stay on drug after 40 weeks
- Strengths included:
- A large sample size
- Parallel investigation of multiple adalimumab biosimilars
- Application of mandatory harmonized monitoring strategy
- Limitations included:
- This study was not designed to support the superiority or noninferiority of biosimilar adalimumab-adaz, nor was it powered to show statistical significance. Endpoints were not prespecified
- A relatively short follow-up time
- The lack of data on fecal calprotectin levels
- ADA serum drug trough levels and ADA measurements were not performed

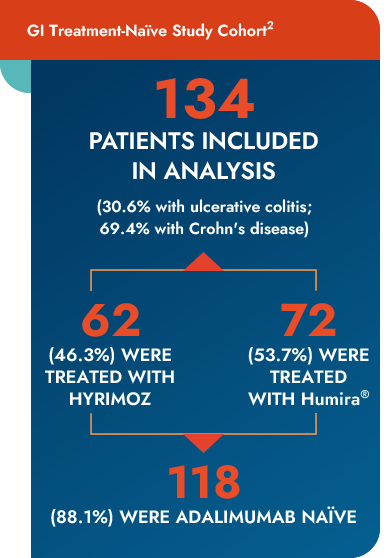
Study design
- A retrospective review of outpatients in an Italian real-life setting
- This analysis enrolled consecutive patients with IBD with complete clinical, laboratory, and endoscopic datab
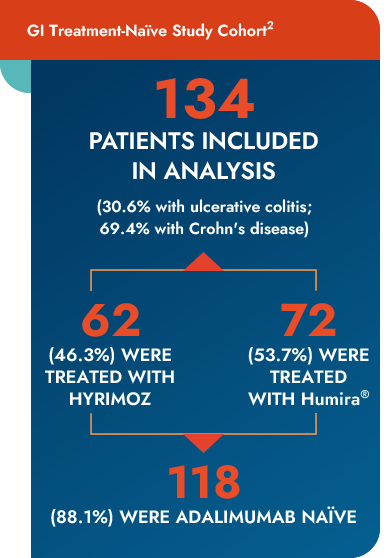
- 134 patients (30.6% with ulcerative colitis and 69.4% with Crohn's disease) were enrolled
- 62 (46.3%) patients were treated with biosimilar adalimumab-adaz and 72 (53.7%) with reference adalimumab; 118 (88.1%) patients were adalimumab naïvec
Study objective
- The primary endpoints were the induction of remission and the safety of biosimilar adalimumab-adaz vs reference adalimumab
bPatients with mild severity were included, although the indication for biosimilar adalimumab-adaz is for moderate-to-severe ulcerative colitis and Crohn's disease.
cFor patients new to adalimumab, both biosimilar adalimumab-adaz and reference adalimumab were administered subcutaneously at the following doses:160 mg at Week 0, 80 mg at Week 2, and then 40 mg every 2 weeks to maintain remission. For patients previously treated with reference adalimumab who switched to biosimilar adalimumab-adaz, a dose of 40 mg was administered subcutaneously every 2 weeks to maintain remission after switch. Dose optimization (40 mg/week) was required by 9 (6.7%) patients in total; 7 (11.3%) patients in the biosimilar adalimumab-adaz group and 2 (2.8%) in the reference adalimumab group, with a trend toward difference.
bPatients with mild severity were included, although the indication for biosimilar adalimumab–adaz is for moderate-to-severe ulcerative colitis and Crohn's disease.
cFor patients new to adalimumab, both biosimilar adalimumab-adaz and Humira® were administered subcutaneously at the following doses:160 mg at Week 0, 80 mg at Week 2, and then 40 mg every 2 weeks to maintain remission. For patients previously treated with Humira® who switched to biosimilar adalimumab-adaz, a dose of 40 mg was administered subcutaneously every 2 weeks to maintain remission after switch. Dose optimization (40 mg/week) was required by 9 (6.7%) patients in total; 7 (11.3%) patients in the biosimilar adalimumab-adaz group and 2 (2.8%) in the reference adalimumab group, with a trend toward difference.
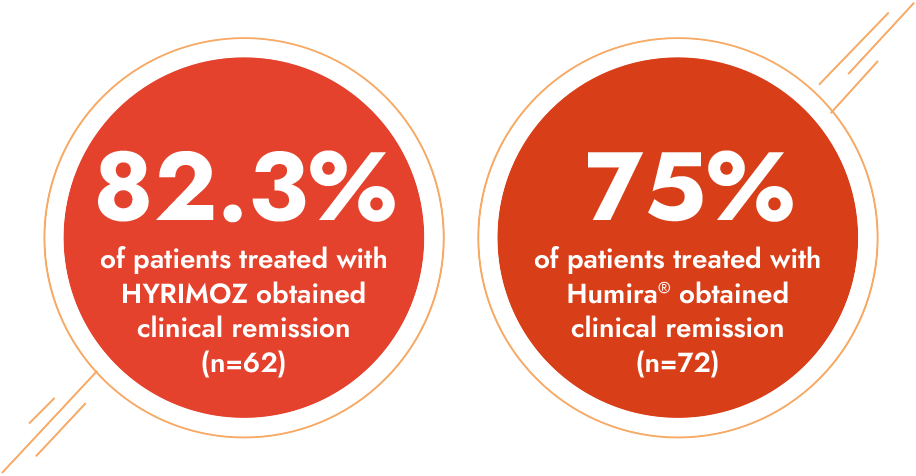
- Clinical remission was obtained in 105 (78.4%) patients during a median follow-up of 12 months
- 82.3% in the biosimilar adalimumab-adaz group
- 75% in the reference adalimumab group
- Treatment was comparable in both groups
- Strengths included:
- Multicenter design, allowing for regional distribution across Italy
- Limitations included:
- This study was not designed to support the superiority or noninferiority of biosimilar adalimumab-adaz, nor was it powered to show statistical significance. Endpoints were not prespecified
- Retrospective nature of the study
- Small sample size
- Relatively short duration of follow-up
- Inconsistent timing for follow-up (clinical and endoscopic)

Dermatology

The Sensoready® pen

Co-pay as low as $0
INDICATIONS: HYRIMOZ® (adalimumab-adaz) injection for subcutaneous use, a prescription medication, is a tumor necrosis factor (TNF)-blocker indicated for:
- Rheumatoid Arthritis (RA): Alone or in combination with methotrexate or other non-biologic disease-modifying anti-rheumatic drugs (DMARDs), for reducing signs and symptoms, inducing major clinical response, inhibiting the progression of structural damage, and improving physical function in adult patients with moderately to severely active RA
- Juvenile Idiopathic Arthritis (JIA): Alone or in combination with methotrexate for reducing signs and symptoms of moderately to severely active polyarticular JIA in patients 2 years of age and older
- Psoriatic Arthritis (PsA): Alone or in combination with non-biologic DMARDs, for reducing signs and symptoms, inhibiting the progression of structural damage, and improving physical function in adult patients with active PsA
- Ankylosing Spondylitis (AS): Reducing signs and symptoms in adult patients with active AS
- Crohn’s Disease (CD): Treatment of moderately to severely active CD in adults and pediatric patients 6 years of age and older
- Ulcerative Colitis (UC): Treatment of moderately to severely active UC in adult patients
Limitations of use: The effectiveness of adalimumab products has not been established in patients who have lost response to or were intolerant to TNF blockers. - Plaque Psoriasis (Ps): Treatment of adult patients with moderate to severe chronic Ps who are candidates for systemic therapy or phototherapy, and when other systemic therapies are medically less appropriate. HYRIMOZ should only be administered to patients who will be closely monitored and have regular follow-up visits with a physician
- Hidradenitis Suppurativa (HS): Treatment of moderate to severe HS in adult patients
- Uveitis: Treatment of non-infectious intermediate, posterior, and panuveitis in adult patients
IMPORTANT SAFETY INFORMATION:
WARNING: SERIOUS INFECTIONS and MALIGNANCY
SERIOUS INFECTIONS
Patients treated with adalimumab products, including HYRIMOZ, are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.
Discontinue HYRIMOZ if a patient develops a serious infection or sepsis.
Reported infections include:
- Active tuberculosis (TB), including reactivation of latent TB. Patients with TB have frequently presented with disseminated or extrapulmonary disease. Test patients for latent TB before HYRIMOZ use and during therapy. Initiate treatment for latent TB prior to HYRIMOZ use
- Invasive fungal infections, including histoplasmosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis, and pneumocystosis. Patients with histoplasmosis or other invasive fungal infections may present with disseminated, rather than localized, disease. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. Consider empiric anti-fungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness
- Bacterial, viral, and other infections due to opportunistic pathogens, including Legionella and Listeria
Carefully consider the risks and benefits of treatment with HYRIMOZ prior to initiating therapy in patients with chronic or recurrent infection.
Monitor patients closely for the development of signs and symptoms of infection during and after treatment with HYRIMOZ, including the possible development of TB in patients who tested negative for latent TB infection prior to initiating therapy.
MALIGNANCY
Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers including adalimumab products. Post-marketing cases of hepatosplenic T-cell lymphoma (HSTCL), a rare type of T-cell lymphoma, have been reported in patients treated with TNF-blockers including adalimumab products. These cases have had a very aggressive disease course and have been fatal. The majority of reported TNF blocker cases have occurred in patients with Crohn's disease or ulcerative colitis and the majority were in adolescent and young adult males. Almost all these patients had received treatment with azathioprine or 6-mercaptopurine (6–MP) concomitantly with a TNF blocker at or prior to diagnosis. It is uncertain whether the occurrence of HSTCL is related to use of a TNF blocker or a TNF blocker in combination with these other immunosuppressants.
WARNINGS AND PRECAUTIONS
Serious Infections
- Do not start HYRIMOZ during an active infection, including localized infections
- If an infection develops, monitor carefully, and stop HYRIMOZ if infection becomes serious. Drug interactions with biologic products: A higher rate of serious infections has been observed in RA patients treated with rituximab who received subsequent treatment with a TNF blocker. An increased risk of serious infections has been seen with the combination of TNF blockers with anakinra or abatacept, with no demonstrated added benefit in patients with RA. Concomitant administration of HYRIMOZ with other biologic DMARDs (eg, anakinra or abatacept) or other TNF blockers is not recommended based on the possible increased risk for infections and other potential pharmacological interactions
- Patients 65 years of age and older, patients with co-morbid conditions and/or patients taking concomitant immunosuppressants may be at greater risk of infection
- Invasive fungal infections: For patients who develop a systemic illness on HYRIMOZ, consider empiric antifungal therapy for those who reside or travel to regions where mycoses are endemic
Malignancies
- In clinical trials, incidence of malignancies was greater in adalimumab-treated patients than in controls
- Consider the risks and benefits of TNF blocker-treatment, including HYRIMOZ, prior to initiating therapy in patients with known malignancy
- Non-melanoma skin cancer (NMSC) was reported during clinical trials for adalimumab-treated patients. Examine all patients, particularly those with a history of prolonged immunosuppressant or PUVA therapy for the presence of NMSC prior to and during treatment with HYRIMOZ
- In the adalimumab clinical trials there was an approximate 3-fold higher rate of lymphoma than expected in the general US population. Patients with chronic inflammatory diseases, particularly those with highly active disease and/or chronic exposure to immunosuppressant therapies, may be at a higher risk than the general population for the development of lymphoma, even in the absence of TNF blockers
- Post-marketing cases of acute and chronic leukemia have been reported in association with TNF-blocker use. Approximately half of the post-marketing cases of malignancies in children, adolescents, and young adults receiving TNF blockers were lymphomas; other cases represented a variety of different malignancies and included rare malignancies usually associated with immunosuppression and malignancies that are not usually observed in children and adolescents
Hypersensitivity Reactions
- Anaphylaxis or serious allergic reactions have been reported following administration of adalimumab products. If an anaphylactic or other serious hypersensitivity reaction occurs, immediately discontinue administration of HYRIMOZ and institute appropriate therapy
Hepatitis B Virus Reactivation
- Use of TNF blockers, including HYRIMOZ, may increase the risk of reactivation of hepatitis B virus (HBV) in patients who are chronic carriers. Some cases have been fatal
- Evaluate patients at risk for HBV infection for prior evidence of HBV infection before initiating TNF blocker therapy
- Exercise caution in patients identified as carriers of HBV and closely monitor during and after HYRIMOZ treatment
- In patients who develop HBV reactivation, stop HYRIMOZ and initiate effective anti-viral therapy. Exercise caution when resuming HYRIMOZ after HBV treatment
Neurologic Reactions
- Use of TNF-blocking agents, including adalimumab products, has been associated with rare cases of new onset or exacerbation of central nervous system and peripheral demyelinating disease, including multiple sclerosis (MS), optic neuritis, and Guillain-Barré syndrome
- Exercise caution when considering HYRIMOZ for patients with these disorders; discontinuation of HYRIMOZ should be considered if any of these disorders develop
- There is a known association between intermediate uveitis and central demyelinating disorders
Hematological Reactions
- Rare reports of pancytopenia, including aplastic anemia, have been reported with TNF-blocking agents. Medically significant cytopenia has been infrequently reported with adalimumab products
- Consider stopping HYRIMOZ if significant hematologic abnormalities occur
Heart Failure
- Worsening and new onset congestive heart failure (CHF) has been reported with TNF blockers. Cases of worsening CHF have also been observed with adalimumab products; exercise caution and monitor carefully
Autoimmunity
- Treatment with adalimumab products may result in the formation of autoantibodies and, rarely, in the development of a lupus-like syndrome. Discontinue treatment if symptoms of a lupus-like syndrome develop
Immunizations
- Patients on HYRIMOZ should not receive live vaccines
- Pediatric patients, if possible, should be brought up to date with all immunizations prior to initiating HYRIMOZ therapy
- Adalimumab is actively transferred across the placenta during the third trimester of pregnancy and may affect immune response in the in utero exposed infant. The safety of administering live or live-attenuated vaccines in infants exposed to adalimumab products in utero is unknown. Risks and benefits should be considered prior to vaccinating (live or live-attenuated) exposed infants
ADVERSE REACTIONS
The most common adverse reactions (incidence >10%): infections (eg, upper respiratory, sinusitis), injection site reactions, headache, and rash.
Please see full Prescribing Information for HYRIMOZ, including Boxed Warning and Medication Guide.
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.




